A*STAR NEWS
PRESS RELEASES
Scientists grow miniature brains that mimic the major pathological features of Parkinson’s disease
- Recreating major pathological features of Parkinson’s disease in a lab-grown, human mini- brain will help researchers to explore new treatments.
- This is the first time that Lewy bodies, a hallmark of Parkinson’s disease in patients’ brains,
have been produced in the laboratory, offering new insights into the disease.
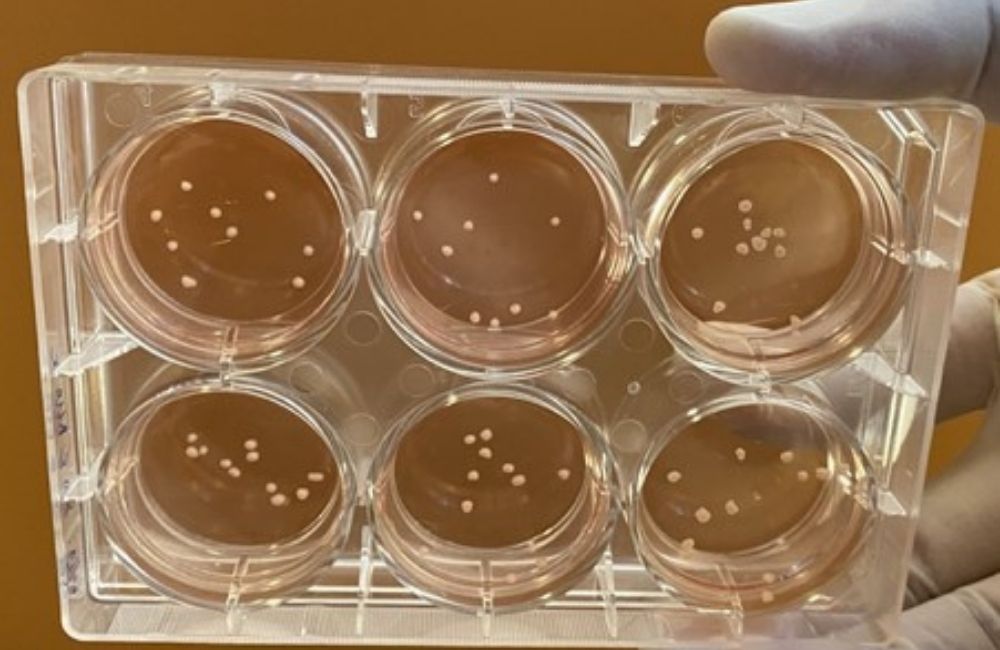 Small pea-sized human midbrain-like organoids – which are essentially three- dimensional, multicellular, in vitro tissue constructs that mimic the human midbrain – are grown from human stem cells to enable scientists to study how the human brain develops and
communicates.
Small pea-sized human midbrain-like organoids – which are essentially three- dimensional, multicellular, in vitro tissue constructs that mimic the human midbrain – are grown from human stem cells to enable scientists to study how the human brain develops and
communicates.
Credit: Associate Professor Hyunsoo Shawn Je, Duke-NUS Medical School
SINGAPORE, 7 September 2021 – Tiny brains-in-a-dish that mimic the major pathological features of Parkinson’s disease have been made for the first time. The research, led by scientists from the Agency for Science, Technology and Research (A*STAR)’s Genome Institute of Singapore (GIS), the National Neuroscience Institute (NNI) and Duke-NUS Medical School, published in the Annals of Neurology, offers a new way to study how the degenerative brain disease progresses and explore possible new treatments.
Parkinson’s disease is a common age-related neurodegenerative disorder affecting three in 1,000 Singaporeans aged 50 years and above. Worldwide, neurological disorders are the leading cause of disability, and Parkinson’s disease is the fastest growing disorder. Prior research has mostly relied on mice, which do not reproduce all major pathological features seen in patients.
“Recreating models of Parkinson’s disease in animal models is hard as these do not show the progressive and selective loss of neurons that produce the neurotransmitter dopamine, a major feature of Parkinson’s disease,” said Prof Ng Huck Hui, Senior Group Leader at GIS, A*STAR, who is a senior co-author of the study. “Another limitation is that experimental mouse models of Parkinson’s disease do not develop characteristic clumps of proteins called Lewy bodies, which are often seen in the brain cells of people with Parkinson’s disease and a type of progressive dementia known as Lewy body dementia.”
The team decided to turn to human mini-brains that they created previously.
“We called these ‘human midbrain-like organoids’,” said first author Dr Junghyun Jo, previously a Research Fellow at GIS and now a Principal Investigator at the Okinawa Institute of Science and Technology Graduate University. “They are essentially three-dimensional, multicellular, in vitro tissue constructs that mimic the human midbrain.”
The small pea-sized human midbrain-like organoids are grown from human stem cells into a bundle of neurons and other cells found in the brain. The organoids enable scientists to study how the human brain develops and communicates.
“These experiments are the first to recreate the distinctive features of Parkinson’s disease that we see only in human patients,” said Associate Professor Hyunsoo Shawn Je, a senior co-author from the Neuroscience and Behavioural Disorders Programme at Duke-NUS. “We have created a new model of the pathology involved, which will allow us to track how the disease develops and how it might be slowed down or stopped.”
By manipulating the DNA of the starting stem cells to match genetic risk factors found in patients with Parkinson’s disease, the study scientists were able to grow organoids with neurons that showed both Lewy bodies and the progressive loss of dopamine-producing neurons.
“It’s a major challenge to extend healthy living years in an ageing global population, whose physical and cognitive performance often declines due to neurodegenerative disorders,” said Professor Tan Eng King, Deputy Medical Director, Academic Affairs, at NNI, a senior co-author of the study. “This discovery provides insights and a ‘humanised’ disease model that can facilitate drug testing against Parkinson’s disease and dementia. Our organoid model with a genetic mutation on the GBA gene is also highly relevant as we have several of these genetic mutation carriers locally.”
The organoid system will enable research into Parkinson’s disease and other conditions not possible with current animal models. The team is already using organoids to investigate why and how Lewy bodies form in human brain cells, and screen drugs that can potentially stop disease progression.
Reference: Jo, J., Yang, L., Tran, H., Yu, W., Sun, A., & Chang, Y. et al. (2021). Lewy Body-like Inclusions in Human Midbrain Organoids Carrying Glucocerebrosidase and α-Synuclein Mutations. Annals Of Neurology. https://doi.org/10.1002/ana.26166
About Duke-NUS Medical School
Duke-NUS is Singapore’s flagship graduate entry medical school, established in 2005 with a strategic, government-led partnership between two world-class institutions: Duke University School of Medicine and the National University of Singapore (NUS). Through an innovative curriculum, students at Duke-NUS are nurtured to become multi-faceted ‘Clinicians Plus’ poised to steer the healthcare and biomedical ecosystem in Singapore and beyond. A leader in ground-breaking research and translational innovation, Duke-NUS has gained international renown through its five signature research programmes and nine centres. The enduring impact of its discoveries is amplified by its successful Academic Medicine partnership with Singapore Health Services (SingHealth), Singapore’s largest healthcare group. This strategic alliance has spawned 15 Academic Clinical Programmes, which harness multi-disciplinary research and education to transform medicine and improve lives.
For more information, please visit www.duke-nus.edu.sg
About A*STAR’s Genome Institute of Singapore (GIS)
The Genome Institute of Singapore (GIS) is an institute of the Agency for Science, Technology and Research (A*STAR). It has a global vision that seeks to use genomic sciences to achieve extraordinary improvements in human health and public prosperity. Established in 2000 as a centre for genomic discovery, the GIS pursues the integration of technology, genetics and biology towards academic, economic and societal impact, with a mission to "read, reveal and write DNA for a better Singapore and world".
Key research areas at the GIS include Precision Medicine & Population Genomics, Genome Informatics, Spatial & Single Cell Systems, Epigenetic & Epitranscriptomic Regulation, Genome Architecture & Design, and Sequencing Platforms. The genomics infrastructure at the GIS is also utilised to train new scientific talent, to function as a bridge for academic and industrial research, and to explore scientific questions of high impact.
For more information about GIS, please visit www.a-star.edu.sg/gis.
About the National Neuroscience Institute (NNI)
The National Neuroscience Institute (NNI) is the national specialist and regional centre of care for the brain, spine, nerve and muscle. NNI offers Neurology, Neurosurgery and Neuroradiology services with advanced technology and multi-disciplinary care teams. Committed to improving patients’ lives, NNI aims to shape neuroscience for a better tomorrow through innovation, research and education. NNI is a member of the Singapore Health Services (SingHealth) – a public healthcare cluster which manages four hospitals, five specialty centres, eight polyclinics and a network of community hospitals.
For more information, visit www.nni.com.sg.
Was This Article Helpful?
A*STAR celebrates International Women's Day

From groundbreaking discoveries to cutting-edge research, our researchers are empowering the next generation of female science, technology, engineering and mathematics (STEM) leaders.
Get inspired by our #WomeninSTEM