FACES OF A*STAR
Opening new perspectives in treatment of metabolic diseases
Dr. S. Sendhil Velan, Head of the Metabolic Imaging Group at A*STAR’s SBIC, and Prof. Johan G. Eriksson, Professor at Yong Loo Lin School of Medicine, Department of Obstetrics and Gynecology at NUS, and Director at A*STAR’s SICS, contributed an editorial to Asia-Pacific Biotech News (APBN) on the topic of metabolic diseases.
The authors highlighted how obesity and Type 2 diabetes are becoming a significant financial and social burden. They also shared how advanced imaging technologies such as magnetic resonance imaging (MRI) and magnetic resonance spectroscopy (MRS) are powerful tools for body composition assessment, which can help researchers and clinicians investigate metabolic diseases and address unmet medical needs.
Left to right: Dr. S. Sendhil Velan, Head of Metabolic Imaging Group, A*STAR’s SBIC (left) with Associate Professor Teoh Yee Leong, CEO of Singapore Clinical Research Institute (centre); and Dr Eveline Bruinstroop, Research Fellow, Duke-NUS Medical School. The findings of the clinical study led by the research team, brings us closer to finding a cure for NAFLD, a major health problem, characterised by the build-up of fat in the liver that is not caused by heavy drinking..
Metabolic Diseases a Global Health Problem
Obesity and Type 2 diabetes are contributing to the global epidemic of metabolic diseases. Their rapidly growing prevalence is a significant financial burden. According to the Diabetes Atlas published in 2017 by the International Diabetes Federation, global health care costs dedicated to treating diabetes and its complications amounted to US$727 billion in 2017. Around 425 million people have diabetes, and this number will increase by over 40 per cent to around 629 million by 2045. Obesity has been identified as a major risk factor for Type 2 diabetes - a chronic condition characterised by resistance to the action of insulin, and impairment in pancreatic insulin secretion; and it is associated with devastating health complications such as cardiovascular disease and chronic kidney disease.
In particular, childhood obesity is a serious global public health challenge. In 40 years, the number of children and adolescents with obesity has risen more than 10-fold; in addition, an even higher number of children has been classified as being overweight. A similar trend has been reported in adults, there are 1.9 billion overweight adults, while 650 million are living with obesity. Among adults, obesity has nearly tripled over four decades.
In Singapore, metabolic disorders also pose an alarming health threat. Modern lifestyles, an urban environment and high nutritional intakes have given rise to an increase in obesity, and related metabolic dysfunctions in Singaporean children and adults. The prevalence of Type 2 diabetes has increased and one in nine Singaporeans has been diagnosed with Type 2 diabetes, and the prevalence of pre-diabetes or impaired glucose tolerance (IGT) is even higher. In the age group 60 to 69 years, almost one in three adults has Type 2 diabetes.
There is an urgent need to identify and implement effective strategies to detect, treat, manage, and prevent these metabolic diseases. The Singapore government is ramping up efforts on a number of fronts, including research and development to find new and better ways to address the growing metabolic disease burden, such as spurring the development of technologies to identify early markers of impairment in glucose metabolism.
Ethnic Differences and Early Life Factors Contribute to Metabolic Diseases
Studies have shown that health and disease are programmed early in life by developmental pathways, and in many cases already during prenatal life. Notably, Asians have major challenges with metabolic dysfunctions including insulin resistance at younger ages, gestational diabetes and Type 2 diabetes occurring at lower degrees of obesity and developing these conditions at younger ages compared to the Caucasian population.
The studies indicate that ethnic differences in metabolism could be driven by genetic factors, and early interventions may be required to prepare a healthy in utero environment, to combat obesity and improve metabolism.
Against this backdrop, academia, the research community, clinical community and industry in Singapore have been working closely, to investigate metabolic diseases and address unmet medical needs. They are drawing upon advanced imaging technologies such as magnetic resonance imaging (MRI) and magnetic resonance spectroscopy (MRS).
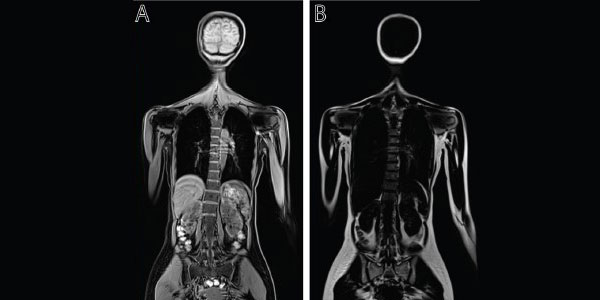
The Figure above shows a representative MR image of water (A) and fat (B) distribution (vertical plane) of a subject. MRI can be utilised quantitatively to assess various adipose tissues including white adipose tissue (WAT) and brown adipose tissue (BAT). WAT is distributed across the body and stores fat whereas BAT present in supraclavicular, paravertebral, and perirenal areas and can help in increasing energy expenditure (Sun L et al., Obesity, 2019). The study of BAT has received great interest especially in the prevention and treatment of obesity. Ectopic fat which accumulates in liver, pancreas, heart and muscle are known to cause lipotoxicity and insulin resistance. It has also been suggested that accumulation of fat in the liver is symptomatic of dysfunctions in glucose metabolism.
MRI and MRS - Gold Standards for Body Composition Assessment
Body mass index (BMI) has traditionally been utilised in clinical settings to evaluate obesity in children and adults. However, BMI as a marker of obesity is not optimal, as it does not provide an accurate measurement of body composition. Quantitative MRI and MRS can overcome this limitation, as they are powerful tools for body composition analysis, and capture comprehensive information on structure, function and metabolism of the human body and brain.
In a clinical study led by a collection of research entities, including A*STAR (Agency for Science, Technology and Research)'s Singapore Bioimaging Consortium (SBIC), Duke-NUS Medical School and the Singapore Clinical Research Institute (SCRI), researchers at SBIC used MRI and MRS to understand the relationship between the thyroid hormone and the metabolism of fatty acids in functional organs of patients with non-alcoholic fatty liver disease (NAFLD). Results from the study showed that low dose thyroid hormone supplementation may be beneficial for reducing fatty liver in male diabetic patients with NAFLD. The findings also affirmed MRI and MRS as gold standards for assessing body composition and measuring metabolic activity. These technologies will support future clinical studies in NAFLD, a major health problem which affects more than 30 percent of Singaporeans.
Such non-invasive imaging modalities are safe, accurate and reliable for longitudinal studies. Over the last few years, A*STAR has established magnetic resonance (MR) imaging strategies for quantitative assessment of various fat depots in children and adults, in Singaporean cohort studies such as the Singapore Adult Metabolism Study (SAMS), which assessed ethnic differences in the predisposition to metabolic diseases such as diabetes and obesity; and GUSTO, a nation-wide birth cohort study, which studies how the conditions in pregnancy and early childhood influence the health and development of women and children.
Our studies with the SAMS cohort and ongoing studies focusing upon the GUSTO cohort clearly highlight the differences in body fat partitioning and insulin sensitivity among different ethnic groups. The multi-ethnic diversity in Singapore adds to the complexity of lifestyle and nutrition which are culturally inherited. These findings signal a need for interventions tailored specifically for each ethnic group.
Advancing Metabolic Imaging in Future Clinical Research Studies
Metabolic imaging will largely increase our knowledge about the pathophysiology of metabolic diseases including obesity, Type 2 diabetes and related metabolic dysfunctions.
Repeated measurements could be performed to evaluate response to pharmacological, nutritional and exercise interventions. Imaging results can also be combined with blood chemistry and genetics, contributing to further development of more targeted approaches for disease treatment and prevention.
In addition to supporting ongoing national research initiatives, we aim to embark on studies into the factors contributing to high-risk pregnancy, through foetal MR imaging, imaging of the pancreas and assessment of insulin secretion as well as assessment of the effects of early diet and exercise interventions among women who experience high-risk pregnancy.
Rapid advancements in metabolic imaging, are generating novel technologies such as hyperpolarised13C MR Imaging, an emerging molecular imaging method that enables rapid, non-invasive, investigation of pathway-specific metabolic and physiological processes that cannot be achieved by conventional imaging, and which will support therapeutic interventions.
Through A*STAR SBIC’s advanced metabolic imaging program, we aim to bring this state-of-the-art technology to Singapore, to drive investigation of metabolism, and support clinical trials in South East Asia.
The potential of imaging techniques in predicting health and disease is immense. As we continue to pursue research and development to investigate major public health issues, we look forward to forging strategic partnerships with the academia, industry, and clinical community, which will help unlock greater possibilities from imaging modalities that impact health care and improve lives.
Was this article helpful?
A*STAR celebrates International Women's Day

From groundbreaking discoveries to cutting-edge research, our researchers are empowering the next generation of female science, technology, engineering and mathematics (STEM) leaders.
Get inspired by our #WomeninSTEM