A*STAR NEWS
atopic dermatitis the search for answers
The National Atopic Dermatitis Research Programme aims to discover the underlying causes of the common but complex skin disorder.
Atopic Dermatitis (AD), commonly referred to as eczema, is an inflammatory skin disorder that results in a dry, itchy, red rash. The condition typically starts in childhood, but can occur at any age. For many patients, AD is a chronic condition that they struggle with for an entire lifetime. More than just a simple skin rash, AD can cause intense itching, pain, loss of sleep, and mental health issues such as anxiety and depression. Treatments also weigh heavily on the patient in terms of time, energy and money.
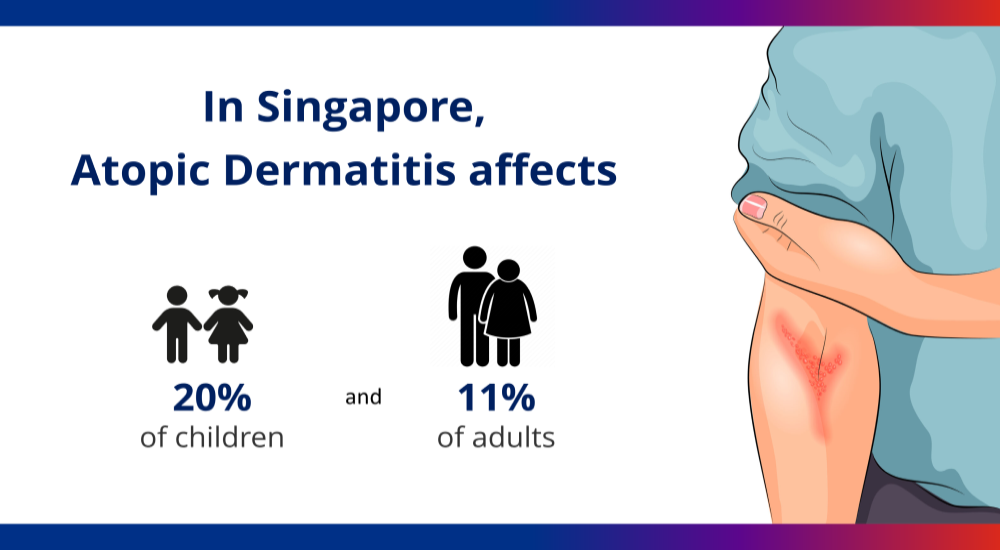
AD is the most common skin disorder in Singapore, affecting an estimated 20 per cent of Singaporean children and 11 per cent of adults. It represents a large clinical burden, with the National Skin Centre alone seeing more than 18,000 cases in 2017. Globally, AD appears to have a similar prevalence in developed countries.
Unfortunately for millions of AD sufferers worldwide, there is currently no known cure for the disorder although increasingly, there are a good number of therapies and drugs. AD is typically diagnosed based on physical examination of the rash, and treatments are focused on reducing the severity and frequency of the symptoms.
outcome-driven research in atopic dermatitis
The Skin Research Institute of Singapore (SRIS)’ National Atopic Dermatitis Research Programme brings together leading researchers, dermatologists, industry partners and end-users to study the multiple facets of AD. SRIS is a tripartite collaboration between the Agency for Science, Technology and Research (via its A*STAR Skin Research Labs, or A*SRL), the National Healthcare Group (NHG), and Nanyang Technological University (NTU).
The National Atopic Dermatitis Research Programme aims to improve health outcomes of this chronic disease and establish Singapore as one of the global leaders in AD research..
To understand the epidemiology, health burden and systems biology of AD in Singapore, the programme is building a cohort of at least 2,000 AD patients and 2,000 controls. Using a combination of clinical, genomic, transcriptomic, and imaging data collected from the cohort, the programme will allow better understanding of the Asian AD pathogenesis, and targeted treatments.
 Scientists work alongside clinicians and dermatologists to understand the underlying causes of AD and develop novel therapies specifically for Asian patients.
Scientists work alongside clinicians and dermatologists to understand the underlying causes of AD and develop novel therapies specifically for Asian patients.
Through in-depth studies of the skin barrier and microbiome, immunology, and itch, researchers are working to identify novel biomarkers, drug targets and potential intervention strategies. To facilitate a comprehensive approach to treating the disease, researchers are also developing novel patient engagement tools, and next-generation diagnostics tools that will enable clinicians to prognosticate disease progression and offer a more effective, tailored treatment approach.
The programme aims to improve health outcomes of this chronic disease - reducing the numbers affected by severe AD by 30 per cent, and reducing the prevalence of AD by 10 per cent by 2023 - and establish Singapore as one of the global leaders in AD research.
“This is a very exciting initiative that draws on expertise from diverse disciplines to understand the Asian-specific AD skin phenotype to enable development of more customised treatments for those effected,” says Dr Leah Vardy, Covering Executive Director of A*SRL.
new insights into the role of skin microbiome
A recent study led by Dr John Common, a Principal Investigator with the A*STAR Skin Research Labs (A*SRL), has discovered different skin microbiome signatures that may suggest why some cases of atopic dermatitis (AD) are more severe than others. These findings provide the first evidence that intrinsic skin microbiome states can be used for stratification and prognostication in AD.
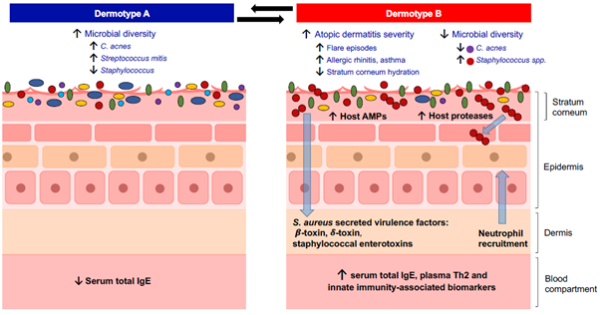 Graphic illustrations of the defining characteristics of Dermotype A and B
Graphic illustrations of the defining characteristics of Dermotype A and B
The researchers identified two microbiome states, which they termed Dermotypes A and B, in the microbial signatures of National Skin Centre patients. Dermotype B is associated with severe itching and frequent flares, shows reduced microbial richness, altered metabolic capacity, and enrichment of virulence genes on the skin. This altered microbial ecology could be a mechanism for driving ongoing systemic inflammation and increased disease severity.
“The ability to manipulate the skin microbiome has great promise for treating skin diseases," says Dr Common. “It raises the possibility that alteration of one’s dermotype state could reduce disease susceptibility and improve barrier function.”
a multi-faceted disease
The pathogenesis of AD involves a complex interplay of multiple factors. Apart from skin microbiome, other factors include skin barrier dysfunction, dysregulation of the immune system, genetic predisposition, and environmental factors.
Dr Common explains this complex interaction: When you have a dry, broken skin as is often the case in AD, the disrupted skin barrier enables allergens and irritants from the environment to penetrate and stimulate the skin.
“Skin surface microbes, pathogens, and allergens, get in and stimulate the immune system, leading to redness in the skin,” he says. “You also get intense pruritus , because when you stimulate the immune system, it releases cytokines that communicate with sensory nerves that are responsible for the itching sensation
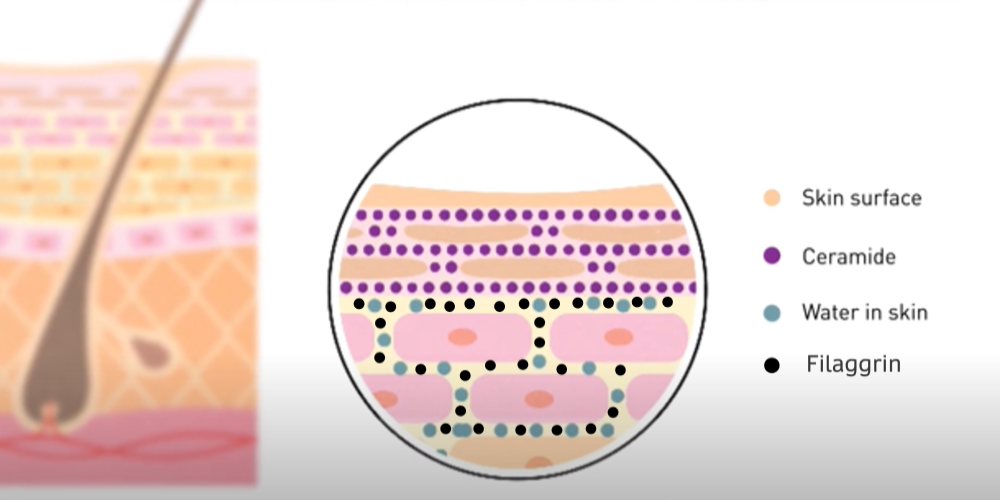 Proteins like filaggrin and lipids such as ceramides, are important for the composition and function of the skin barrier. The lipid and protein barrier prevents water loss from the skin, and the penetration of allergens and pathogens.
Proteins like filaggrin and lipids such as ceramides, are important for the composition and function of the skin barrier. The lipid and protein barrier prevents water loss from the skin, and the penetration of allergens and pathogens.
A number of things - skin barrier disruption, immune activation, and nerve stimulation - are interlinked.
"That makes AD a fascinating disease to study scientifically because it impacts a number of different mechanisms within the skin. We therefore realised that due to the many different facets of AD in the disease cycle, we needed to have a more connected programme to study this in a way that is collaborative and synergistic," he adds.
Innovative treatments for Atopic Dermatitis
 | New biologic drug for AD developed by AslanPharmaceuticals, is currently in clinical trials performed by SRIS and NSC. The therapeutic antibody known as ASLAN004 can inhibit proteins that are key to triggering eczema symptoms such as redness and itchiness. Initial results coming out were very promising. |
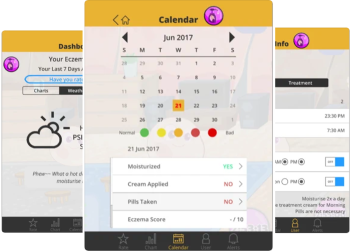 | AD Programme: App (Taggle Eczema) to monitor atopic dermatitis in patients for personalised AD treatment and better patient management and compliance. |
 | The AD programme in SRIS, together with the Institute of Chemical and Engineering Sciences, is collaborating with local SME Hyphens Pharmaceuticals to formulate and clinically validate a hand cream for AD patients with dry skin. |
Was This Article Helpful ?
A*STAR celebrates International Women's Day

From groundbreaking discoveries to cutting-edge research, our researchers are empowering the next generation of female science, technology, engineering and mathematics (STEM) leaders.
Get inspired by our #WomeninSTEM